EcoTipping Points
- How do they work?
- Leveraging vicious
cycles to virtuous - Ingredients for success
- Create your own
EcoTipping Points!
Stories by Region
- USA-Canada
- Latin America
- Europe
- Middle East
- South Asia
- Southeast Asia
- East Asia
- Africa
- Oceania-Australia
Stories by Topic
- Agriculture
- Business
- Education
- Energy
- Fisheries
- Forests
- Public Health
- Urban Ecosystems
- Water and Watersheds
Short Videos
- Saving a Coral Reef and Fishery (Apo Island, Philippines)
- Community Gardens Reverse Urban Decay (NYC, USA)
- Community Forests Reverse Tropical Deforestation (Thailand)
- Escaping the Pesticide Trap (India)
- Rainwater Harvesting and Groundwater Replenishment (Rajasthan, India)
How Success Works:
- Saving a Coral Reef and Fishery (Apo Island, Philippines)
- Community Gardens Reverse Urban Decay (NYC, USA)
- Community Forests Reverse Tropical Deforestation (Thailand)
- Escaping the Pesticide Trap (India)
- Rainwater Harvesting and Groundwater Replenishment (Rajasthan, India)

Human Ecology:
Principles underlying
EcoTipping Points
Vietnam - Dengue Hemorrhagic Fever, Copepods, and Biological Control of Mosquitoes
- Author: Gerry Marten
- This in-depth story is from Human Ecology: Basic Concepts for Sustainable Development (Gerald Marten, Earthscan Publications, 2001), pages 184-196, available online: Chapter 12 at www.gerrymarten.com/human-ecology/tableofcontents.html
- Watch: One-minute video clip of Macrocyclops albidus preying upon first-instar Aedes albopictus larvae
The story of Dengue Hemorrhagic Fever, an “emergent” disease known only since 1950, illustrates the benefits that are possible with local community action and ecological management. Dengue Hemorrhagic Fever is transmitted by mosquitoes that breed in water storage tanks and other water-filled containers around people’s homes. There is no vaccine or medicine for this virus; the only way to prevent the disease is to get rid of the mosquitoes. Initially spectacular success controlling the mosquitoes with DDT during the 1950s and 1960s was not sustainable because the mosquitoes evolved resistance to DDT. Other pesticides have gone into use, but there has been no overall reduction in the disease. Nearly one hundred million people in tropical Asia and Latin America are infected with dengue each year, about one-half million children are afflicted with life-threatening Dengue Hemorrhagic Fever, and thousands die. The pesticide-based strategy of the last fifty years has been a failure, but what else can be done? Ecological management promises to be more effective and sustainable. The copepod Mesocyclops provides an example. This tiny crustacean kills virtually all the mosquito larvae whenever it is in water-filled containers where mosquitoes breed. Vietnam has mounted a campaign to distribute Mesocyclops throughout the country. The mosquito and the disease have disappeared from every village that uses Mesocyclops, the key to success being strong community organization to ensure that everyone uses the copepods.
The disease and the mosquito
Dengue is a flavivirus related to yellow fever. It may have originated in non-human primates, which still provide a natural reservoir in Africa and Asia. Non-human primates do not show symptoms, but humans can become seriously ill. First-time dengue infections in children are usually mild and often unnoticed, but first-time infections in adults may be severe. Fatalities are rare, but high fever, chills, headache, vomiting, severe prostration, muscle and bone aches and severe weakness for more than a month after the fever subsides make dengue fever an illness that many adults remember as the worst sickness they ever experienced.
Dengue hemorrhagic fever is a life-threatening form of dengue. It is not caused by a separate viral strain; instead, it comes from the fact that the dengue virus has four distinct strains. Infection with one strain confers lifelong immunity to that strain but also creates antibodies that enhance infection with the other three strains. Dengue hemorrhagic fever typically occurs when infection with one strain is followed a year or more later by infection with another strain. About 3 per cent of second infections produce dengue hemorrhagic fever, and about 40 per cent of dengue hemorrhagic fever cases develop a shock syndrome that can be fatal. The most damaging symptom is fluid leakage from capillaries into tissues and body cavities, sometimes accompanied by severe gastrointestinal bleeding (hence the name hemorrhagic). There is no medicine to counter the virus, but the loss of fluids can be treated by getting water and electrolytes into the vascular system, administered orally in mild cases and intravenously in severe cases. Most dengue hemorrhagic fever victims are under 15 years old. If untreated, about 5 per cent of cases are fatal, but proper treatment can reduce fatalities to less than 1 per cent.

Above: Electron micrograph of a female Mesocyclops. Source: Michael Brown.
The mosquito Aedes aegypti is the principal vector of both dengue and yellow fever. Originally a tree-hole-breeding mosquito in Africa, it long ago acquired an urban life style by breeding in similar situations around human habitations. Aedes aegypti now breeds in man-made containers such as water storage tanks, wells, clogged rain gutters and discarded objects such as tyres, tin cans and jars that collect rainwater. The mosquito lays her eggs on the side of a container a few millimetres above the water level. The eggs can sit for months without hatching if they remain dry, but they hatch within minutes if covered with water. The fact that this normally happens only when more water is added to a container increases the probability that a container will have enough water for the larvae to complete their development before the container dries out.
While male mosquitoes feed only on plant juices, females suck blood from animals to get the nutrients they need to develop their eggs. When a female takes blood from a person infected with dengue, the virus multiplies in her body, and 7 to 15 days later (depending upon temperature) she has enough of the virus to infect people. Transmission of the virus is much higher in tropical climates, where rapid viral multiplication at higher temperatures makes it more likely for an infected mosquito to survive long enough to become infectious.
History of dengue
Starting in the 16th century with the expansion of European colonialism and trade, Aedes aegypti spread around the world by hitching rides in water storage containers on boats. Dengue and Aedes aegypti existed in Asia for centuries without serious consequences because the distribution of Aedes aegypti was limited by Aedes albopictus, an indigenous Asian mosquito that is physiologically capable of transmitting dengue but not associated with significant dengue transmission in practice. Asian towns and cities were well endowed with trees and shrubs, and Aedes albopictus competitively excluded Aedes aegypti wherever there was vegetation.
The situation in the Americas was quite different. Aedes aegypti thrived in cities and towns because no mosquito like Aedes albopictus restricted its distribution. We know Aedes aegypti was common in the Americas because of numerous yellow fever epidemics following the introduction of yellow fever from Africa by the slave trade in the 16th century. The historical record for dengue is not clear because its symptoms do not distinguish it from other diseases, but dengue was probably common throughout much of the Americas for centuries. Philadelphia had a dengue fever epidemic in 1780. Dengue fever was common in towns and cities on the Gulf and Atlantic coasts of the United States until the 1930s.
Dengue probably spread everywhere with Aedes aegypti, but it did not attract much attention, even where the infection rate was high, because most people were infected as children with mild symptoms. Devastating epidemics made yellow fever a very different matter. Aedes aegypti became an object of international attention when Walter Reed demonstrated in 1900 that this mosquito was responsible for yellow fever transmission. Campaigns were initiated in the Americas to get rid of Aedes aegypti by eliminating the places where it bred around people’s houses. During the 1930s the Rockefeller Foundation mobilized a virtual army of house-to-house government inspectors in Brazil to find and eliminate every place Aedes aegypti might breed. Inspectors had legal authority to enter premises, destroy containers, apply oil or paris green (an arsenic mosquito larvicide) and impose fines. It was possible to consolidate the eradication of Aedes aegypti neighbourhood by neighbourhood, without reinvasion, because adult Aedes aegypti usually travels less than 100 metres in a lifetime. The campaign was so effective that Aedes aegypti was eradicated from large areas of Brazil by the early 1940s.
Although there were outbreaks resembling dengue hemorrhagic fever in Queensland, Australia, in 1897 and in Greece in 1928, dengue hemorrhagic fever was not a recognized disease until 1956 because it was unusual to have more than one strain in the same region. Everything changed with World War II, when large numbers of people and the four dengue strains were moved around the Asian tropics. There were numerous dengue fever epidemics during the war as the virus was introduced to new areas where people lacked immunity. Cases with dengue hemorrhagic fever symptoms appeared in Thailand in 1950. The first recognized dengue hemorrhagic fever epidemic was in the Philippines in 1956, followed by epidemics in Thailand and other parts of South-East Asia within a few years. Uncontrolled growth of developing world cities during the following decades greatly expanded Aedes aegypti’s breeding habitat. Urban landscapes provided a bounty of water storage tanks and discarded containers collecting rainwater in neighbourhoods lacking basic services such as piped water and trash collection. The decline of vegetation in urban landscapes allowed Aedes aegypti to expand through Asian cities without competition from mosquitoes such as Aedes albopictus.
The spread of dengue hemorrhagic fever was probably delayed by the appearance of DDT in 1943. DDT was like a miracle. It was harmless to vertebrates at concentrations used to kill insects, and it was effective for months after application. In 1955 the World Health Organization began a global campaign to spray every house in malarial areas with DDT. Malaria virtually disappeared from many areas by the mid 1960s, and at the same time Aedes aegypti disappeared from most of Latin America and some parts of Asia such as Taiwan.
Failure of the DDT strategy
The incredible success of DDT was short-lived because mosquitoes evolved resistance that spread quickly around the world. Developing world governments could not afford to continue intensive spraying, particularly when alternatives to DDT such as malathion cost more than ten times as much. Malaria started to return in force by the late 1960s, and by the mid 1970s Aedes aegypti returned to most areas from which it had previously been eradicated. Dengue did not return to the United States because window screening and air conditioning led to an indoor life style that reduced contact between people and mosquitoes. However, the four dengue strains and dengue hemorrhagic fever spread rapidly through tropical Asia, settling into a permanent pattern of recurring local dengue fever outbreaks as the four strains continued to circulate. Dengue hemorrhagic fever entered the Americas in 1981 with an epidemic in Cuba that hospitalized 116,000 people in three months. Dengue quickly spread through much of Latin America, sometimes punctuated by dengue fever epidemics of hundreds of thousands of people, but dengue hemorrhagic fever was generally sporadic because most areas had only one strain. Although dengue was common in many parts of sub-Saharan Africa, it was not a major health problem because Africans are generally resistant to severe dengue infection.
The social and political situation for dealing with Aedes aegypti had changed immensely since the campaigns against yellow fever earlier in the century. A few wealthier countries such as Taiwan continued to spray houses with newer insecticides, and a few countries such as Cuba and Singapore initiated comprehensive house inspections and fines to get rid of Aedes aegypti breeding around people’s homes. However, most countries lacked the political will and the financial and organizational resources to implement such programmes. Chemical larvicides that kill all the mosquito larvae, and later a microbial larvicide (Bacillus thuringiensis), were available to treat water storage containers. However, people were reluctant to put pesticides in their water. Even if people are willing, larvicides must be applied on a weekly basis to be effective. The cost of purchasing larvicides and managing large-scale use proved beyond the capacity of every government that tried to implement it. Some governments tried to organize voluntary community participation to eliminate Aedes aegypti breeding habitats – advising housewives, for example, to clean their water storage containers weekly to interrupt development of the larvae – but without much success.

Above: Electron micrograph of Mesocyclops mouth parts. Source: Michael Brown.
There is no vaccine or medicine for dengue; the only way to prevent the disease is to get rid of the mosquitoes. Today the main action against the mosquitoes is by individual families who purchase insecticide spray cans and mosquito coils to keep mosquitoes from bothering them at night. The effect on Aedes aegypti is limited, because this mosquito bites during the day and spends most of its time resting in places such as clothes closets beyond the reach of casual spraying. Vaccine development has been underway for years; but progress has been slow, and a vaccine could be risky because it might enhance susceptibility to dengue hemorrhagic fever, as happens after natural dengue infections. It is now typical in most places for governments to do little about Aedes aegypti until there is a dengue epidemic or dengue hemorrhagic fever appears. Then trucks drive up and down streets spraying malathion, with little impact in many instances because the epidemic is already well underway and female Aedes aegypti are inside houses where not much insecticide can reach them. Even if spraying manages to reduce the mosquito population, it must be repeated frequently to sustain the impact. Aedes aegypti can rebound to large numbers within a few days.
There has been no noticeable decrease in dengue fever or dengue hemorrhagic fever cases during the past 20 years. Worldwide, about 50 to 100 million people are infected with dengue each year. There are several million severe dengue fever cases and about 500,000 dengue hemorrhagic fever cases annually. Fatalities have remained high in some countries, but other countries have reduced fatalities dramatically by providing extensive medical treatment. Several hundred thousand people are hospitalized with dengue hemorrhagic fever in Vietnam and Thailand every year, but the fatality rate is less than 0.3 per cent. Nonetheless, the economic costs are high. Patients require one to three weeks of hospitalization, and parents lose work time while caring for sick children in hospitals. Global warming could eventually extend the geographic range of dengue as higher temperatures, and consequently shorter viral incubation times in mosquitoes, stimulate transmission.
Copepods enter the scene
Although biological control with predators of Aedes aegypti larvae offers the possibility of functioning without the frequently repeated applications necessary for pesticides, it did not receive serious consideration when the DDT strategy collapsed. Fish were widely used against malarial mosquito larvae prior to the DDT era, but the use of fish for Aedes aegypti control was limited because fish were expensive and did not survive for long in most containers. Besides, many people did not want fish in their water storage containers, particularly if they used the water for drinking. Many aquatic animals such as planaria, dragonfly nymphs and aquatic bugs were known to prey on mosquito larvae, but none had ever proved effective enough or practical enough to go into operational use. Mosquito-control professionals and public health officials, who relied heavily on chemical pesticides throughout their careers, considered biological control a pipe dream. Opportunities for profit were too remote to stimulate research and development by the private sector.
This was the situation about 20 years ago, when scientists in Tahiti, Colombia and Hawaii independently discovered that virtually no Aedes larvae survived in water-filled containers if the copepod Mesocyclops aspericornis was present. Copepods are tiny crustaceans that are ecologically very different from other aquatic invertebrates that prey on mosquito larvae. If mosquito larvae are numerous, the copepods eat only a small part of each larva, giving each copepod the capacity to kill 30 to 40 larvae per day, far more than they actually eat. Even more important is their large numbers. Copepods eat small animals up to twice their own size, but they also eat phytoplankton, protozoa and rotifers – a diet that provides enough food to make copepods the most abundant predator in most freshwater habitats. The total capacity of a copepod population to kill mosquito larvae is enormous. Most species of copepods are too small (0.3–1.2 millimetres in body length) to prey on even the smallest mosquito larvae, but Mesocyclops aspericornis and other large species of copepods (1.2 millimetres or more in body length) attack and consume newly hatched mosquito larvae without hesitation. About 10 per cent of areas with water where mosquitoes might breed have natural populations of Mesocyclops or other large copepods, which drastically reduce the survival of mosquito larvae.
Figure 12.1 - Mesocyclops (actual length approximately 1.5 millimetres) Note: Copepods do not have eyes; the eyespot in the middle of the forehead detects light but does not form an image. Copepods move by means of rapid oarlike movements of their large antennules (the long structures extending to each side of the body from the front). The antennules contain mechanical sensory organs that detect vibrations in the water so that copepods know when small animals such as mosquito larvae are close enough to be captured as food. Female copepods carry egg sacs on both sides of their body for about three days until young copepods emerge from the eggs.
The same thing that happens in nature can be achieved by introducing appropriate copepod species to sites that do not already have them. This principle applies not only to containers where Aedes aegypti is breeding but also to aquatic habitats where Anopheles malarial mosquitoes breed. Malarial mosquito larvae are generally scarce in habitats that contain natural populations of large Mesocyclops species; Anopheles larvae disappeared when Mesocyclops were introduced to rice fields and small marsh areas in Louisiana. Unfortunately, the potential of Mesocyclops for malaria control has not been developed further because malaria control agencies have abandoned their efforts to control mosquitoes. Contemporary malaria control is based almost entirely on anti-malarial drugs, whose long-term effectiveness is doubtful due to drug resistance already widespread among malarial parasites.
The development of copepods for dengue control has been much more successful because copepods are effective and easy to use in the simple container habitats where Aedes aegypti breeds. It is unusual for copepods to get into man-made containers on their own; but they thrive in many kinds of containers when introduced, and they do so independently of the supply of mosquito larvae. Copepod populations range from hundreds in a rainwater-filled tyre to thousands in a water storage tank. The largest species usually kill more than 99 per cent of the Aedes aegypti larvae, and they usually stay in a container for as long as there is water. Even without water, they can survive as long as there is moisture.
The simple life cycle of copepods and their ability to thrive on a diet of protozoa make mass production easy and inexpensive. The production system uses bacteria on decomposing wheat seed as food for a small protozoan (Chilomonas) that provides food for young copepods and a larger protozoan (Paramecium caudatum) that provides food for the larger stages. The system is simple, inexpensive and highly resilient, functioning in open containers of any size or shape. One hundred adult female Mesocyclops produce about 25,000 new adult females within a month. Females are inseminated during adolescence and require no further contact with males to produce 50 to 100 eggs weekly during their several-month life span.
Once it was realized how effective copepods are, research was initiated in Australia, South-East Asia and the Americas to identify the best copepod species for mosquito control and how to utilize them. Suitable species were always available locally because copepods large enough to kill mosquito larvae occur naturally virtually everywhere that Aedes aegypti is a problem. Mesocyclops aspericornis is the most effective species in Polynesia, Australia and parts of Asia. Mesocyclops longisetus, the world’s largest species of Mesocyclops, proved most effective in the Americas.
In order for a copepod to be effective at controlling Aedes aegypti, it must do more than kill mosquito larvae. It must also be good at surviving in containers. Mesocyclops aspericornis and Mesocyclops longisetus are good at surviving in sun-exposed containers in the tropics because they tolerate water temperatures up to 43º Celsius. Moreover, because they cling to the bottom and sides of a container, they survive in water storage containers from which people frequently scoop water. Copepods that swim in the water column quickly disappear from a water storage container. Mesocyclops aspericornis and Mesocyclops longisetus are effective in wells, cisterns, cement tanks, 200-litre drums, clay jars, flower vases and even bromeliads if they have water on a continuous basis. People do not object to copepods in their water storage containers because these tiny animals are barely noticeable. Besides, it is not unusual for other small aquatic animals to live in the water.
Copepods do not survive in small rainwater-filled containers or discarded tyres that dry out frequently, though they do well in tyres that are continuously filled with water during the rainy season. They do not survive in small cement tanks with rapid water turnover, particularly if the water is frequently run down the drain, and they are killed when bleach is left in a tank after cleaning or slopped into a tank while washing clothes next to the tank. A significant difficulty is the loss of copepods from water storage containers when they are cleaned. This is easily overcome by saving a small quantity of water from the container to restock it with copepods after cleaning. In small-scale pilot projects in Honduras and Brazil, housewives quickly learned to monitor their containers, maintaining Mesocyclops at their homes with pride. The key to success was personal attention from community organizers. Unfortunately, Latin American public health bureaucracies seem to lack the capacity for neighbourhood organization to expand the use of Mesocyclops on a larger scale.
Success in Vietnam
Dengue hemorrhagic fever is a serious concern in Vietnam because it has hospitalized nearly two million Vietnamese and killed more than 13,000 children since appearing there 40 years ago. The first demonstration of how effective Mesocyclops can be on a community scale began in 1993, when scientists at Vietnam’s National Institute of Hygiene and Epidemiology introduced local species of Mesocyclops into all of the water storage containers in Phanboi, a village of 400 houses in northern Vietnam. Like most of rural Vietnam, the two main sources of Aedes aegypti in Phanboi were large cement tanks (several-thousand litre capacity), which nearly every house uses for long-term storage of rainwater from the roof, and clay jars (20- to 200-litre capacity) used to store water for immediate use. Mesocyclops thrived in the large cement tanks, which are seldom drained or cleaned. They did nearly as well in large clay jars but could not survive for long in small clay jars because the water was frequently poured out. Introduction of Mesocyclops to wells provided a reservoir that continually restocked clay jars used to store well water.
The Aedes aegypti population in Phanboi declined by about 95 per cent during the year after Mesocyclops introduction. However, Aedes aegypti was still breeding in small discarded containers such as jars, bottles and cans that collected rainwater but could not be treated with Mesocyclops. Villagers were encouraged to participate more actively, and motivation was high due to a prior history of dengue hemorrhagic fever outbreaks in the village. The socialist political system provided a basis for rapid, comprehensive and continuous community mobilization. The village women’s union educated villagers about the use of Mesocyclops and organized villagers to stock any containers without Mesocyclops by pouring in a small quantity of water from containers that already had them. An existing recycling programme for discarded containers was reorganized to ensure they did not collect rainwater while waiting for pickup. Aedes aegypti disappeared within a few months, and no Aedes aegypti mosquitoes or their larvae have been sighted in the village during the subsequent seven years. The disappearance of Aedes aegypti was significant because it was the first time in more than 20 years that even a local eradication of any kind of mosquito had been documented anywhere in the world, and it was accomplished without pesticides.
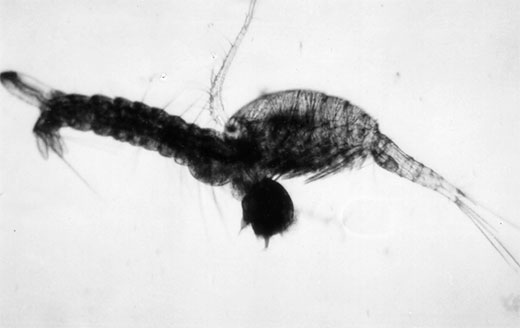
Above: Mesocyclops aspericornis seizing an Ae. aegypti larva.
Watch: One-minute video clip of Macrocyclops albidus preying upon first-instar Aedes albopictus larvae
Mesocyclops was then introduced to other villages in northern Vietnam, and Aedes aegypti disappeared from them as well. It is noteworthy that Aedes aegypti disappeared without having Mesocyclops in every container. Success was probably due to the ‘egg-trap effect’. Egg-laying mosquitoes do not discriminate against containers with Mesocyclops, so they waste their eggs on containers with Mesocyclops instead of putting them in containers with better prospects for larval survival. Computer simulation studies indicate that a mosquito population will collapse if Mesocyclops is in more than 90 per cent of the containers. In contrast, getting rid of 90 per cent of the containers only reduces mosquito populations in the model by 90 per cent.
The successful demonstration at Phanboi was essential for mobilizing official government support and foreign financial assistance to distribute Mesocyclops to more communities in Vietnam. Television publicity and school education programmes are making Mesocyclops a household word. A government inquiry telephone line refers interested communities to health workers who can provide Mesocyclops and explain their use. A simple mass-production system at Vietnam’s National Institute of Hygiene and Epidemiology uses 150-litre plastic waste pails to produce several hundred thousand Mesocyclops per month at very low cost.
The programme follows the Phanboi model. Central staff members train local health workers, who in turn use videotape documentaries to introduce Mesocyclops to the community. The health workers train local teachers to organize students for regular collection of discarded containers. From the village women’s union, health workers recruit volunteer ‘collaborators’ with demonstrated reliability in ongoing house-to-house family planning and immunization programmes. Each collaborator is responsible for 50 to 100 houses and starts by introducing about 50 Mesocyclops into a tank at one of the houses. As soon as the copepods multiply to large numbers, the collaborator carries a bucket of tank water containing Mesocyclops around to all the other houses, pouring a glass of the water into every container. Collaborators explain the use of Mesocyclops to every family and return at least once a month to inspect the containers. The programme has trained about 900 health workers and collaborators, and Mesocyclops has been distributed to more than 30,000 households in northern and central Vietnam.
Most communities in the programme have repeated the scenario at Phanboi. Aedes aegypti disappears about a year after Mesocyclops introduction. The few exceptions have been urban communities, where Aedes aegypti has declined but not disappeared; the reason is incomplete coverage of the houses by local collaborators. It is sometimes necessary to recruit collaborators of unknown reliability in urban areas that lack ongoing house-to-house health programmes. While most new collaborators do a good job, some do not, and their task can be complicated by lower social cohesion in cities. With 12 million Vietnamese households in dengue areas, the potential number to be served is enormous. The bottleneck for national distribution of Mesocyclops is training health workers and local collaborators. Some provinces are setting up their own Mesocyclops production and training centres. The programme will face its greatest challenge as it extends to southern Vietnam, whose tropical climate is ideal for Aedes aegypti and dengue transmission throughout the year.
Transporting large numbers of Mesocyclops from production facilities to villages can be a problem because copepods quickly exhaust their food supply when crowded in a small quantity of water. Then they eat each other. An easy solution comes from the fact that Mesocyclops can survive for months suspended on damp foam rubber, where they cannot move to eat each other. Foam rubber cubes are stacked in small plastic containers for mailing to public health offices throughout Vietnam. The copepods are introduced to a water storage container by dropping a foam rubber cube with 50 copepods into the container.
Vietnam reported 234,000 dengue hemorrhagic fever cases in 1998, responsible for more deaths than any other infectious disease. In 1999 the government initiated a high-priority national dengue programme with Mesocyclops in a leading role, not only for dengue prevention but also for dealing with dengue outbreaks in areas where Mesocyclops is not yet in use. The government provides kits to local health workers for rapid blood analysis of suspected dengue cases so that an immediate emergency response can go into action wherever dengue is confirmed. As the supply increases, Mesocyclops will be routinely distributed to houses in outbreak areas.
Prospects for Mesocyclops in other countries
Can other countries use Mesocyclops as successfully as Vietnam? The prospects are particularly promising in South-East Asia, where dengue hemorrhagic fever is a major health problem, public concern is high and most Aedes aegypti breeding habitats are similar to the water storage containers that have proved ideal for Mesocyclops in Vietnam. Public motivation is not as strong outside of South-East Asia, and some of the breeding habitats are not as ideal for Mesocyclops. While dengue control in other areas will often require substantially more than Mesocyclops and container recycling, Mesocyclops can eliminate Aedes aegypti production from at least some kinds of containers almost everywhere that dengue is a problem.
The mechanics of production and distribution are not an obstacle to extending Mesocyclops to other countries. Production is inexpensive, and shipment to local distributors is easy. While production and distribution in Vietnam is by national, provincial and local government, distribution in other countries could use any combination of governmental department, non-governmental organization and the private sector that works under local conditions. The key to success is community organization. It is straightforward enough to put copepods in containers and restock the containers whenever copepods are lost, but it is essential to make sure that everyone does it. Success can proceed neighbourhood by neighbourhood. 100 houses that work together can free themselves of Aedes aegypti even if houses in the surrounding area do nothing.
The most promising strategy is to distribute Mesocyclops where local networks provide the greatest prospects for success. Vietnam has the advantage that most of its dengue is in rural areas where community organization is strongest and house-to-house health programmes are already functioning well. Fortunately, thousands of communities in other countries also have house-to-house networks of one sort or another for primary health care, family planning, paramedical malaria treatment, agricultural extension, religious charity and small business support. These same networks could serve as vehicles for distributing Mesocyclops and ensuring their proper use on a community scale. Even private marketing networks, which so effectively distribute insecticide spray cans and mosquito coils, could play a role if rewards based on community use are built into the incentive system. With each success, the demonstration effect should stimulate more communities to organize so that they can use Mesocyclops successfully.
Conclusions
What does the dengue hemorrhagic fever case study tell us? Firstly, it shows how human activities create environmental conditions that determine whether a disease will flourish or disappear. International transportation created dengue hemorrhagic fever by moving the four dengue strains around the world. Dengue disappears when people eliminate the opportunities for Aedes aegypti to breed in water-filled containers around their homes.
Secondly, it demonstrates how local mosquito eradication is possible with ecological management. An ecological disease-control strategy that integrates a variety of control methods is more effective than a strategy based exclusively on pesticides. We can expect ecological methods to be sustainable. It is unlikely that mosquito larvae will evolve resistance to Mesocyclops.
Thirdly, it demonstrates the level of effort necessary for success. The effort that prevails nearly everywhere in the world today does not meet that standard. Nor does it meet the standard of the yellow fever campaign that eradicated Aedes aegypti from much of Brazil 60 years ago, a campaign that owed its success to its intensity and its meticulous organization and management.
Finally, and most importantly, it highlights the central role of local community. Dengue hemorrhagic fever will be eliminated only through an intense and well-organized effort at the local level. The general lack of progress with dengue during the past 30 years is not unique. Social support systems in local communities have declined throughout the world as personal and public priorities have shifted in other directions. Numerous dimensions of human welfare that depend upon strong local communities have declined correspondingly. While responsibility for a strong and effective local community must reside primarily with local citizens, encouragement and assistance from national governments can be decisive. Ecologically sustainable development, including sustainable control of mosquito-transmitted diseases, will become a reality only when and where local communities are truly functional.
References
- Brown, M, Kay, B and Hendrix, J (1991) ‘Evaluation of Australian Mesocyclops (Copepoda: Cyclopoida) for mosquito control’, Journal of Medical Entomology, vol 28, pp618–623
- Christophers, S (1960) Aedes aegypti (L.). The Yellow Fever Mosquito: Its Life History, Bionomics and Structure, Cambridge University Press, Cambridge
- Focks, D, Haile, D, Daniels, E and Mount, G (1993) ‘Dynamic life table model for Aedes aegypti (Diptera: Culicideae): analysis of the literature and model development’, Journal of Medical Entomology, vol 30, pp1003–1017
- Halstead, S (1997) ‘Epidemiology of dengue and dengue hemorrhagic fever’ in Gubler, D and Kuno, G (eds) Dengue and Dengue Hemorrhagic Fever, CAB International, New York
- Halstead, S (1998) ‘Dengue and dengue hemorrhagic fever’ in Feigin, R and Cherry, J (eds) Textbook of Pediatric Infectious Diseases, W B Sanders, Philadelphia
- Halstead, S and Gomez-Dantes, H (eds) (1992) Dengue – a worldwide problem, a common strategy, Proceedings of an International Conference on Dengue and Aedes aegypti Community-based Control, Mexican Ministry of Health and Rockefeller Foundation, Mexico
- Marten, G (1984) ‘Impact of the copepod Mesocyclops leuckarti pilosa and the green alga Kirchneriella irregularis upon larval Aedes albopictus (Diptera: Culicidae)’, Bulletin of the Society for Vector Ecology, vol 9, pp1 - 5 Download .pdf (2.64mb)
- Marten, G, Astaeza, R, Suárez, M, Monje, C and Reid, J (1989) ‘Natural control of larval Anopheles albimanus (Diptera: Culicidae) by the predator Mesocyclops (Copepoda: Cyclopoida)’, Journal of Medical Entomology, vol 26, pp624 - 627 Download .pdf (60kb)
- Marten, G (1990) ‘Evaluation of cyclopoid copepods for Aedes albopictus control in tires’, Journal of American Mosquito Control Association, vol 6, pp681 - 688 Download .pdf (960kb)
- Marten, G (1990) ‘Elimination of Aedes albopictus from tire piles by introducing Macrocyclops albidus (Copepoda, Cyclopoida)’, Journal of American Mosquito Control Association, vol 6, pp689 - 693 Download .pdf (530kb)
- Marten, G, Bordes, E and Nguyen, M (1994) ‘Use of cyclopoid copepods for mosquito control’, Hydrobiologia, vol 292/293, pp491 - 496 Download .pdf (490kb)
- Marten, G, Borjas, G, Cush, M, Fernández, E, and Reid, J (1994) ‘Control of larval Ae. aegypti (Diptera: Culicidae) by cyclopoid copepods in peridomestic breeding containers’, Journal of Medical Entomology, vol 31, pp36 - 44 Download .pdf (1.14mb)
- Marten, G, Thompson, G, Nguyen, M and Bordes, E (1997) Copepod Production and Application for Mosquito Control, New Orleans Mosquito Control Board, New Orleans, Louisiana Download .pdf (330kb)
- Marten, G and Reid, J (2007) ‘Cyclopoid copepods’, In Tom Floore (ed), Biorational Control of Mosquitoes, American Mosquito Control Association Bulletin No. 7, pp65-92 Download .pdf (1.14mb)
- Nam, V, Yen, N, Kay, B, Marten, G and Reid, J (1998) ‘Eradication of Aedes aegypti from a village in Vietnam, using copepods and community participation’, American Journal of Tropical Medicine and Hygiene, vol 59, pp657 - 660 Download .pdf (58kb)
- Riviere, F and Thirel, R (1981) ‘La predation du copepods Mesocyclops leuckarti pilosa sur les larves de Aedes (Stegomyia) aegypti et Ae. (St.) polynesiensis essais preliminaires d’utilization comme de lutte biologique’, Entomophaga, vol 26, pp427–439
- Soper, F, Wilson, D, Lima, S and Antunes W (1943) The Organization of Permanent Nation-wide anti-Aedes aegypti Measures in Brazil, The Rockefeller Foundation, New York
- Suarez, M, Ayala, D, Nelson, M and Reid, J (1984) ‘Hallazgo de Mesocyclops aspericornis (Daday) (Copepoda: Cyclopoida) depredador de larvas de Aedes aegypti en Anapoima-Colombia’, Biomedica, vol 4, pp74–76